Overview
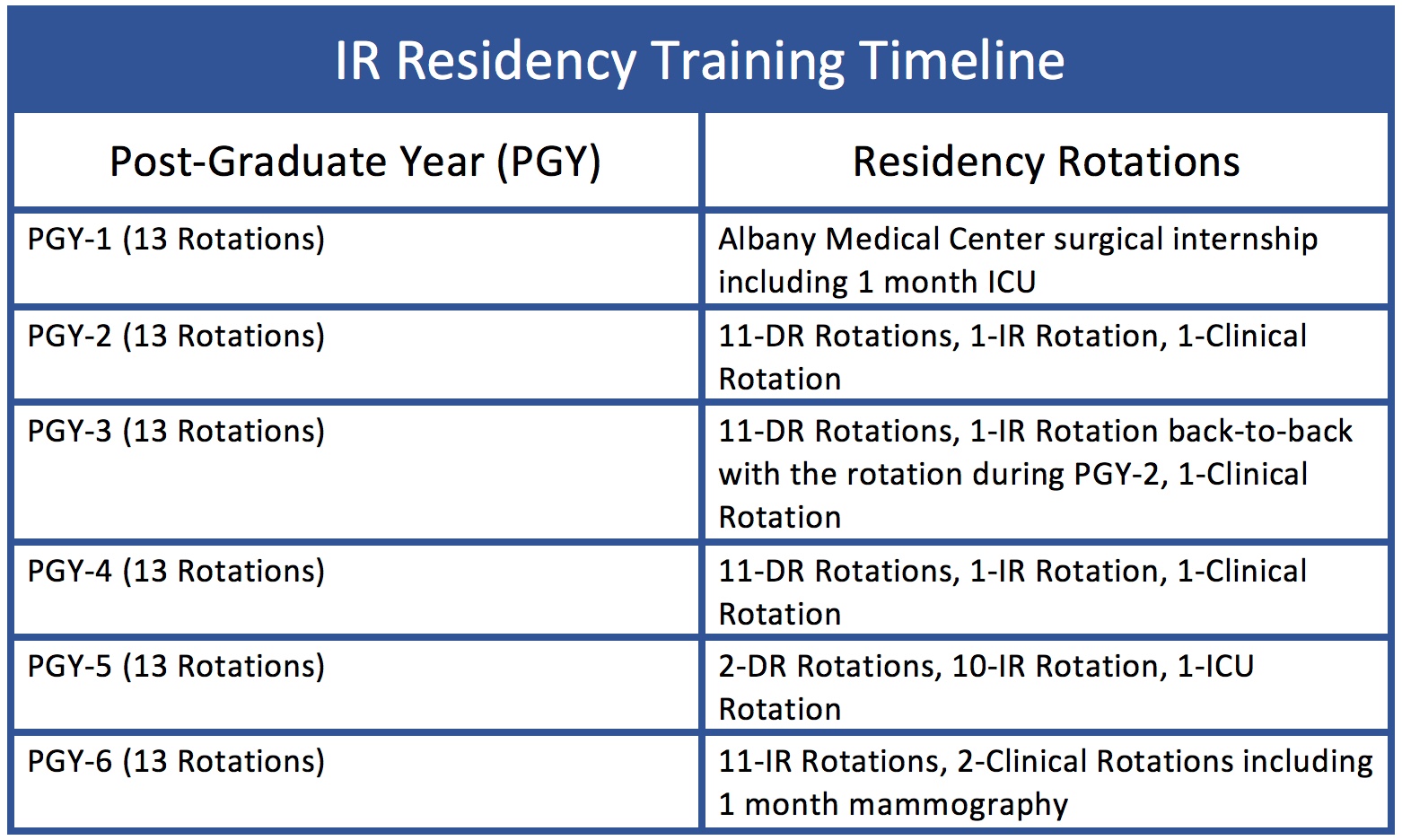
In 2016, we were very proud to earn accreditation for an integrated IR residency at Albany Medical Center. We matched our first resident in March 2017. Click here to learn more about our IR residents. Trainees in this program will spend 6 years with us, including a surgical internship year (PGY-1), three years of diagnostic radiology (PGY-2, PGY-3, and PGY-4), and two years of interventional radiology training (PGY-5 and PGY-6). Moving forward, we will be offering 1 position/year in the IR residency. Please see the chart below outlining the residency training timeline.
For specific information regarding the diagnostic radiology portion of the IR residency, please refer to the information posted on the GME portion of the Albany Medical Center website (click here). As we make some changes in this portion of the training that are specific to the IR residency, we will post them here.
Curriculum
Periprocedural Expertise: The volume of procedures in our division provides each IR resident with an abundance of opportunities to develop and enhance their procedural skills. Our residents will graduate with an enviable proficiency in image-guided procedures and the confidence to bring these abilities to the next step in their careers. However, it is important that our IR residents understand and gain proficiency in the entire episode of care surrounding an IR procedure. Success in this field is achieved when as much attention is paid to the patient before and after the procedure as is paid to the patient during the procedure.
Procedural Training: Individuals pursuing training in interventional radiology require proficiency in a wide spectrum of vascular and nonvascular procedures. The Albany Medical Center IR Residency Program provides trainees with in-depth exposure to the multitude of procedures performed by our specialty, including:
Chemoembolization (TACE)
Radioembolization (Y-90)
Percutaneous cryoablation, microwave ablation, and radiofrequency ablation
Women's interventions
Trauma interventions (AMC is a Level I trauma center)
Embolization
Stenting
Biliary interventions
Percutaneous transhepatic cholangiography and biliary stenting
Perctuaneous cholecystostomy tube placement
Liver disease and portal hypertension
Transjugular interahepatic shunt (TIPS)
Balloon retrograde transvenous obliteration (BRTO)
Genitourinary interventions
Percutaneous nephrostomy tube placement
Nephroureteral stenting
Suprapubic catheter placement
Gastrointestinal interventions
Gastrostomy and gastrojejunostomy tube placement
Gastrointestinal bleeding embolization
Pain interventions
Pediatric interventions
Venous access
Biopsies
Drainages
Deep venous thrombosis and pulmonary embolism thrombolysis
Chronic venous disease
Varicose veins
Inferior vena cava filter placement
Venous access
Dialysis catheter placement
Hemodialysis fistula/graft interventions
Renal biopsies
Abdominal aortic aneurysm endoleak embolization
Biopsies and drainages
Program Structure
Hospital-Based Experience: Now that we have fully transitioned to the IR residency, we typically have one PGY-5 (junior resident) and one PGY-6 (chief resident) on the IR service at any one time. There is also one diagnostic radiology resident on the service at all times. In an effort to fairly distribute the clinical responsibilities and procedural volume between the junior resident and chief resident, there are two roles assigned on a daily basis: procedure resident and clinical resident. The "procedure resident" position is meant to be procedural in nature. As a result, this resident gets to choose the procedures they are going to perform on that day. This position, however, is not limited to simply performing procedures. It is expected that the procedure resident will manage the entire episode of care surrounding the procedure for each patient they are treating. This means that the procedure resident is responsible for morning rounds presentations, pre-procedure consultations, post-procedure orders (including admission orders if applicable), and rounding on the patients undergoing procedures he/she performs or intends to perform. It is our intention to have the resident assigned to this role select the procedures they are going to perform on a given day but this may not be the case periodically in order to balance the experience among all of the residents on the IR service. The "clinical resident" position is primarily responsible for managing the IR clinical service. This means rounding on patients previously seen by IR and evaluating requests for consultations. Other members of the IR team, including our junior residents, medical students, and nurse practitioners, share these responsibilities. It is expected that the clinical resident help coordinate the efforts made by all members of the team towards successful completion of these responsibilities. The clinical resident should participate in procedures at those times during the day when their clinical responsibilities have been completed.
Office-Based Experience: An important component of the experience gained during this residency is the time spent in our outpatient office. In the context of this clinic, residents evaluate new patients prior to therapeutic procedures, see patients in follow-up and perform office-based procedures. The practice of interventional radiology has changed significantly during the past several years, and the outpatient office has been an integral part of that change. By moving from a hospital-based specialty to an office-based specialty with hospital privileges, the field of IR has evolved. Interventional radiologists have moved from just providing care to patients during a procedure to providing care throughout an entire episode of care for a patient. This means assuming responsibility for evaluating patients before procedures, performing procedures, and following patients after procedures. Much of those responsibilities are carried out at our outpatient office. Each resident in the IR program will spend one day/week in our outpatient office at the Capital Region Health Park in Latham, NY during their PGY-5 and PGY-6 years. As diagnostic radiology residents during the PGY-2 through PGY-4 years, we will also create opportunities for observation in the IR office. The day of the week spent in the office will change on a monthly basis during the PGY-5 and PGY-6 years so that each IR resident is given the opportunity to spend consistent time with one attending in their office (since each attending's office has a slightly different focus).
Responsibilities
Procedural Responsibilities: When it comes to performance of procedures, we have created a system whereby graded responsibility is given to each resident during the final two years (PGY-5 and PGY-6 years) of the residency program (the "IR" years). Early on in the PGY-5 year, procedures are performed under direct supervision, with an attending physician in the room, scrubbed into the procedure with the resident. It is expected that the residents gain an understanding of the assistant role during procedures and must be proficient with that role before moving onto the role of primary operator. This typically involves understanding the indications for the procedure, the instruments on the table, the table side controls of the equipment, and the role of the nurse and technologist within the procedure room. It is also essential that residents demonstrate the ability to anticipate the next steps in a procedure before they occur. Residents should demonstrate these abilities and this knowledge through active interaction with the attendings before, during, and after procedures. As comfort is gained with the procedural skill of each individual resident, attendings will begin to permit limited independent performance of all or part of certain procedures. This will be at the discretion of the individual attending responsible for individual procedures. It is our hope that our residents will be able to perform most procedures independently by the mid-end of the PGY-5 year. It is also expected that residents demonstrate an understanding of limiting both radiation exposure and contrast administration with patient safety in mind. Ultimately, it is a combination of technical proficiency and judgement that will enable residents to gain procedural independence during the residency.
On-Call Responsibilities: It is anticipated that the junior resident and chief resident will take call approximately 1-2 weeknights/week and no more than 1 in 3 weekends. The chief resident takes slightly less call than the junior resident in a given year. The diagnostic radiology resident rotating on IR takes call 1 weeknight/week and 1 weekend/month. The resident on call is responsible for taking the initial calls for any procedure or patient care issues that arise during off-hours. All procedure requests and urgent issues regarding patients on the IR service should be discussed with the attending on-call. At times, it may be appropriate for the resident to come in and evaluate a patient prior to calling in staff and at other times, staff should be called in while the patient is being evaluated in order to expedite the procedure. Albany Medical Center is a level I trauma center and expectations for responsiveness are an important part of that designation. The on-call responsibilities for IR residents almost never require staying in-house over night. If that becomes necessary, on-call rooms are provided.
Teaching Responsibilities: Our IR residents are expected to participate in teaching diagnostic radiology residents and medical students rotating on the IR service. The diagnostic radiology resident is expected to help with evaluations of inpatient cases and to be actively involved in procedures. However, each of these residents may have different degrees of interest in being involved with procedures; they are encouraged though to be involved in as many cases as possible. It is expected that the IR residents help manage the role that the diagnostic radiology resident has while rotating on IR. The IR residents can delegate a portion of their responsibilities to the diagnostic radiology resident(s) rotating on IR but not all of their responsibilities. Sometimes it is the interaction that the IR residents have with the diagnostic radiology residents that shapes the way they think about interventional radiology; we want their impressions to be positive. At times, medical students spend time rotating on IR. The IR residents should play a role in medical student education as well, introducing them to the field of IR and giving them insight into the procedural and peri-procedural care provided by our service. The chief IR resident has the responsibility of organizing a quarterly M&M conference and journal club.
Goals & Objectives
Overall Program Goals
The goal of the IR residency program is to have our trainees provide patient care through safe, efficient, appropriately utilized, quality-controlled diagnostic and/or interventional radiology techniques. At the conclusion of residency training, the trainee will be able to:
Understand the essential components of direct patient management during an entire episode of care surrounding performance of an image-guided procedure, including pre-procedure assessment and post- procedure management in both the inpatient and outpatient setting.
Understand the criteria used to select patients for image-guided procedures based on history, physical examination, imaging studies, laboratory analysis, and proposed/expected procedural outcomes.
Understand the interaction that interventional radiologists must have with other specialties to provide comprehensive patient care.
Understand the interaction that interventional radiologists must have with the member of the IR team (nurses, technologists, mid-level providers, secretaries) to successfully care for patients.
Understand the clinical presentation, diagnosis, treatment, and long-term management of the vascular and nonvascular disease processes commonly encountered and treated by interventional radiologists.
Demonstrate technical proficiency in the performance of image-guided procedures commonly performed by interventional radiologists.
Understand the importance of ongoing quality improvement initiatives within interventional radiology with the goals of improving patient safety, reducing errors, and improving patient outcomes.
Competency-Based Objectives
Patient Care: Residents must demonstrate an ability to provide patient care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. By the end of the year, residents will be expected to:
Evaluate a patient prior to an image-guided procedure in the inpatient or outpatient setting with preparation of a thorough consultation that includes a history, physical examination, review of medications, lab studies, and imaging studies, and the formation of an assessment and plan.
Obtain informed consent from a patient after discussing the potential risks and benefits of a proposed procedure and alternative therapeutic options.
Competently perform all medical and invasive procedures considered essential for the practice of Interventional Radiology.
Demonstrate the appropriate utilization of sterile technique during invasive procedures.
Identify factors from a patient’s history, physical examination, and laboratory values that allows for the assignment of an ASA score to indicate potential risk for conscious sedation.
Identify factors from a patient’s history, physical examination, and laboratory values that indicate potential risks for bleeding, cardiovascular problems, respiratory abnormalities, renal injury, and adverse drug interactions during or after an interventional procedure.
Supervise physiologic monitoring before, during, and after image-guided procedures and recognize the abnormalities and physical signs/symptoms that require immediate attention during a procedure.
Administer and maintain effective moderate sedation/analgesia for patient comfort during and after an interventional procedure.
Demonstrate an understanding of how to manage certain pharmacological considerations surrounding the performance of image-guided procedures (e.g., drug/contrast reactions, antibiotic therapy, moderate sedation, analgesia, anticoagulation, blood pressure, diabetes management).
Provide appropriate patient follow-up in the inpatient and outpatient setting with effective communication to referring physicians.
Recognize and treat complications that may potentially arise during and after image-guided procedures (e.g., contrast/anaphylactic reaction, over-sedation, pain, nausea/vomiting, decreased oxygen saturation, hypertensive urgency/emergency, low blood pressure, hyper-hypoglycemia or bleeding/hematoma).
Demonstrate an understanding of radiation exposure during image-guided procedures. Residents must be able to apply radiation safety principles in performing interventional procedures and are expected to:
Identify the types of radiation created and their sources during fluoroscopy.
Identify the organs especially sensitive to the effects of ionizing radiation and the maximum yearly whole body dose.
Understand how radiation exposure is monitored.
Understand the principles and practical applications of radiation protection.
Understand the rationale for lead protective clothing, lead glasses, shields and gloves.
Identify periodic maintenance and maintenance schedules for radiation protection.
Understand methods to decrease radiation dose to the patient and operator during IR procedures.
Demonstrate an understanding of the risk of occupational injury during the performance of image-guided procedures. Specifically, residents should be able to:
Describe how to limit/reduce work related musculoskeletal injuries in the IR environment. - Identify patients at high risk for blood borne pathogens.
Know the incidence of hepatitis-C in the IR patient population
Describe methods to reduce accidental exposure to blood and body fluids in the IR suite.
Medical Knowledge: Residents must demonstrate knowledge about established and evolving biomedical, clinical, epidemiological and social-behavioral sciences and the application of this knowledge to patient care. By the end of the year, residents will be expected to:
Engage in continuous learning and apply appropriate state of the art diagnostic and/or interventional radiology techniques to meet the clinical needs of the patients, referring physicians, and the health care system.
Demonstrate that they read IR-related textbooks and journals in the context of their training.
Attend weekly didactic lectures in Interventional Radiology and participate in topic-based discussions at the weekly IR Residents conference.
Attend and actively participate in multidisciplinary conferences (such as GI tumor board).
Attend national Interventional Radiology conferences.
Actively participate in IR-related research projects leading to presentation and/or publication at local, regional, national, or international meetings.
Practice-Based Learning and Improvement: Residents must be able to investigate, evaluate, and improve patient care practices. By the end of the year, residents will be expected to:
Locate, appraise, and assimilate evidence from scientific studies related to their patients’ health problems.
Apply knowledge of study designs and statistical methods to the appraisal of clinical studies and other information on diagnostic and therapeutic effectiveness.
Attend and actively participate in Interventional Radiology Morbidity and Mortality Conference and the Interventional Radiology Quality Improvement Meeting with the goal of systemically analyzing the quality of IR practice.
Facilitate the learning of students and other health care professionals.
Use information technology to manage patient care, access on-line medical information, and support one’s own education and the education of diagnostic radiology residents and medical students.
Interpersonal and Communication Skills: Residents must demonstrate interpersonal and communication skills that result in effective information exchange and teaming with patients, their patients’ families, and professional associates. By the end of the year, residents will be expected to:
Work effectively with others as a member or leader of a health care team or other professional group.
Effectively coordinate on-call emergency procedures.
Demonstrate the ability to dictate timely and appropriate reports for diagnostic imaging studies and interventional radiology procedures.
Effectively communicate with referring physicians and consultants regarding procedure appropriateness and potential risks that require further evaluation prior to performance of an image-guided procedure.
Effectively communicate with patients and their families in a caring manner regarding the medical conditions being treated, the image-guided procedures being performed, and how these procedures t into an overall treatment plan.
Professionalism: Residents must demonstrate a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population. By the end of the year, residents will be expected to:
Demonstrate a commitment to high standards of professional conduct, including altruism, compassion, honesty, and integrity.
Follow principles of ethics and confidentiality and consider religious, ethnic, gender, educational, and other differences in interacting with patients and other members of the health care team.
Demonstrate a commitment to excellence and on-going professional development.
Comply with institutional and departmental requirements (dress code, wearing and submitting radiation badges, displaying ID, etc.)
Serve as a role model for residents and medical students.
Demonstrate a willingness to perform additional duties that contribute to the overall patient care and academic interests of the section.
Systems-Based Practice: Residents must demonstrate an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value.
Understand how the components of the local and national healthcare system function independently and how changes to improve the system involve group and individual efforts.
Understand the systems used for procedure coding (CPT) and diagnosis coding (ICD9) for the billing of procedural services in interventional radiology.
Practice cost-effective health care and resource allocation that does not compromise quality of care.
Consult with other healthcare professionals and educate healthcare consumers regarding the most appropriate utilization of imaging resources.
Demonstrate a willingness to partner with health care managers and health care providers to assess, coordinate, and improve health care and know how these activities can affect system performance.
The Interventional Radiology Residency Program at Albany Medical Center is fully accredited by the Accreditation Council for Graduate Medical Education (ACGME). The department of radiology participates in the National Residency Matching Program (NRMP). Applications for the interventional radiology residency are only accepted through the Electronic Residency Application Service (ERAS). The residency match timeline can be found on the NRMP website.
Application Process
Contact
For more information or to ask questions about the IR residency, please contact Rachelle Stepnowski, our residency coordinator for Interventional Radiology, at (518) 262-2397 or by email at rstepnowski@communitycare.com.